EMDR vs. CBT: Which Therapy is Right for You?
Two proven therapies, two different paths—let’s help you pick the one that fits your brain, your life, and your goals.
Key Takeaways
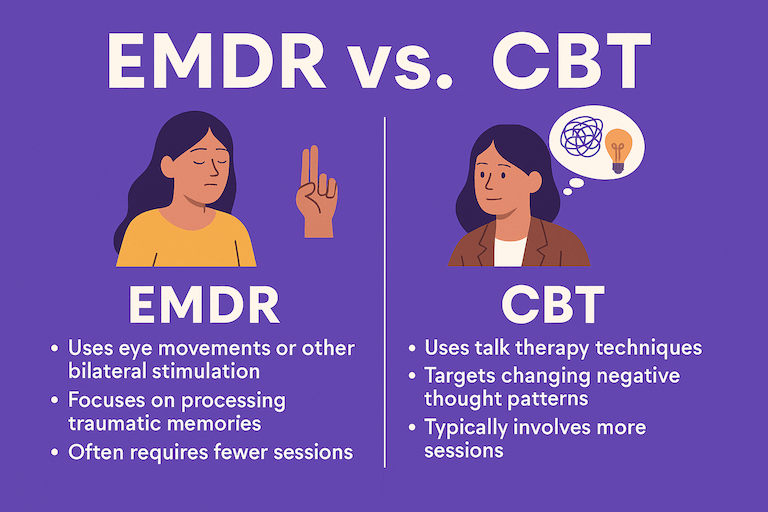
EMDR and CBT are both evidence-based—they just take different routes to relief, offering distinct pathways to recovery. EMDR reprocesses distressing memories with bilateral stimulation; CBT teaches skills to change unhelpful thoughts and behaviors. Both are considered effective treatments for a range of mental health issues. EMDR and CBT are among the primary treatment options for trauma and anxiety, and both are designed to help people heal from psychological distress. Get the basics of EMDR: Understanding EMDR
Choose EMDR when trauma, painful memories, or stuck body responses drive your symptoms (PTSD, panic after a scare, medical trauma, grief with intrusive imagery). See: EMDR for PTSD and Panic Attacks and Grief & Loss
Choose CBT when day-to-day patterns keep anxiety or mood going—like catastrophic thinking, avoidance, or habits you can retrain (GAD worry, social anxiety, insomnia, depression). For OCD, CBT with ERP is first-line; EMDR can help with trauma that fuels obsessions. CBT is a therapeutic approach rooted in cognitive restructuring and behavioral techniques. Read: EMDR for OCD.
Mix-and-match is common. Many people do EMDR for the “stuck” stuff and CBT for skills, relapse prevention, or exposure. Telehealth works for both:
Kids and teens can do both, but the approach is adapted (more play/visuals for EMDR; simplified, hands-on skills for CBT). See: EMDR for Children & Teens.
Bottom line: If your symptoms feel tied to specific memories, lean EMDR. If they’re mostly present-day habits and thoughts, lean CBT. Not sure? A good clinician will help you decide after a brief assessment.
Key difference: CBT often requires homework assignments to practice new skills, while EMDR focuses primarily on in-session work. The key differences between EMDR and CBT lie in their techniques, theoretical foundations, and how each method uniquely addresses trauma and mental health issues.
EMDR vs. CBT: Side-by-Side Comparison
| Aspect | EMDR Trauma-focused | CBT Skills-focused |
|---|---|---|
| Primary goal | Reprocess “stuck” memories so triggers lose their charge and beliefs shift to adaptive ones. | Identify and change unhelpful thoughts/behaviors with structured skills and practice. |
| Best for | PTSD, complex trauma, single-incident trauma, panic tied to events, grief, some phobias. | General anxiety/worry, depression, OCD (with ERP), insomnia, social anxiety, skills coaching. |
| Core techniques | Bilateral stimulation (eye movements/taps/tones), eight-phase protocol, past-present-future targets. | Cognitive restructuring, behavioral experiments, exposure exercises, coping skills & homework. |
| Session focus | Briefly activate a memory/trigger while grounded; let the brain complete processing. | Collaborative discussion, worksheets, skill drills, planning and reviewing at-home practice. |
| Typical timeline | Often 6–12 sessions for a single event; longer for complex histories; intensives possible. | Usually 8–20+ weekly sessions depending on goals and severity; steady skill-building. |
| Homework load | Light—tracking reactions, using calming tools; brief logs. | Moderate to high—thought records, exposures, habit practice between sessions. |
| What it feels like | Less talking; more internal processing. Many feel emotions move and settle during sets. | Active coaching and problem-solving; practical and highly structured. |
| Evidence base | Strong for PTSD and trauma-related symptoms; growing for panic, phobias, grief. | Extensive for anxiety, depression, OCD (ERP), insomnia, panic, phobias, and more. |
| Works well with | CBT/skills training, mindfulness, medication, family involvement. | EMDR for trauma roots, medication, mindfulness, group programs. |
| Not ideal when | Acute instability without safety/coping skills; severe dissociation without stabilization. | Strong trauma triggers derail practice; insight is high but memories remain highly charged. |
| Good fit if you say… | “I keep seeing that image.” “It’s over but doesn’t feel over.” “Talking hasn’t moved it.” | “I overthink and avoid.” “I want a plan & step-by-step tools.” “I’m ready for exposures.” |
| Example outcomes | Triggers lose intensity; sleep and startle improve; beliefs shift (e.g., “I’m safe now”). | Less worry/rumination; consistent coping routines; improved mood and functioning. |
| Access & coverage | Widely available; billed as psychotherapy; many plans cover EMDR with licensed clinicians. | Very widely available; typically in-network for most plans; group options can reduce cost. |
Meet the Methods
What is EMDR (Eye Movement Desensitization and Reprocessing)?
EMDR was originally developed to help trauma survivors process distressing experiences. EMDR helps your brain reprocess distressing memories so they feel in the past-happening now, addressing past traumas that continue to affect mental health. In each therapy session, you briefly notice a target (image, sensation, belief) while doing bilateral stimulation (eye movements, taps, or tones). Unlike traditional talk therapy, EMDR relies less on verbal expression and more on these techniques to facilitate healing. Over sets, distress drops and more balanced beliefs stick. EMDR sessions typically last 60 to 90 minutes and include specific phases for effective processing of trauma, guided by an emdr therapist.
Best for: trauma/PTSD, panic after a specific scare, phobias with a clear starter memory, grief images, medical/dental trauma, performance blocks during/after an incident, cumulative first-responder/military stress.
You don’t have to tell every detail. Processing can be non-graphic and titrated, as EMDR can target a traumatic memory without requiring full disclosure.
EMDR therapy involves eight phases to help clients process and reframe traumatic memories. In the preparation phase, the emdr therapist teaches specific techniques to manage emotional responses and ensures you are ready for the process. The EMDR process addresses both past memories and present disturbances that arise during sessions.
Learn how a session flows: What to Expect in EMDR.
More on complex histories: EMDR for Complex PTSD & Childhood Trauma and Dissociation & Stabilization
What is CBT (Cognitive Behavioral Therapy)?
CBT is rooted in cognitive therapy, which focuses on analyzing ingrained thought and behavior patterns. CBT teaches practical skills to change unhelpful thoughts and ingrained behavior patterns, as well as avoidance. You’ll learn to spot thinking traps, test them with experiments, practice exposure (gradual facing of fears), and build new habits (sleep, activity, communication). These are known as CBT interventions and are tailored to individual needs. CBT sessions are structured and can vary in length, typically spanning multiple weeks depending on individual needs.
Best for: generalized anxiety/worry, social anxiety, depression, insomnia, health anxiety, and OCD (with ERP)
Active and structured: expect homework, logs, and step-by-step plans.
External primers: APA on CBT and IOCDF on ERP for OCD.
“CBT is like strength training for your brain—reps build resilience. EMDR is like surgery for stuck memories—quick, focused, and relieving.”
EMDR vs. CBT at a Glance
How they work:
EMDR: Reprocesses memories and body responses; less talking, more neuroprocessing. Uses distinct pathways focused on memory processing.
CBT: Reshapes thoughts/behaviors with skills, exposure, and practice. Follows distinct pathways centered on cognitive restructuring.
Speed:
EMDR: Often faster for single-event trauma. Research has found significant differences in how quickly EMDR can reduce symptoms compared to CBT for certain issues.
CBT: Steady, skill-building; speed varies by practice and complexity. Significant differences in effectiveness may depend on the type of problem treated.
Homework:
EMDR: Light (grounding, sleep care).
CBT: Moderate to high (exposure steps, thought logs).
Talking about trauma:
EMDR: Minimal detail needed.
CBT: More discussion and planning, especially for exposure.
Telehealth: Both adapt well online. See:
Which Works Best…For What?
PTSD & Trauma
Go EMDR when intrusive images, nightmares, startle, and body jolts dominate. It reduces the “then-is-now” feeling quickly. Both EMDR and CBT are effective for treating PTSD, especially when symptoms stem from a traumatic event or multiple traumatic events such as accidents, war, or sexual assault.
Add CBT for sleep skills, communication, or relapse plans. These therapies help process psychological trauma and address the emotional and cognitive impact of such experiences. PTSD often co-occurs with other disorders like depression and anxiety, so comprehensive treatment is important.
Learn more: EMDR for PTSD
General education: Cleveland Clinic EMDR overview
Anxiety & Panic
EMDR if a clear scare “flipped the switch” (crash, medical event, bad trip, lockdown). Both EMDR and CBT are effective for treating anxiety symptoms, making them valuable options for individuals experiencing PTSD and related conditions.
CBT (with interoceptive exposure) for ongoing fear of sensations and anticipatory anxiety. CBT is also widely used for substance abuse treatment, helping clients address addictive behaviors and develop healthier thought patterns.
Phobias
EMDR can neutralize the starter memory (the bite, turbulence, stuck elevator).
CBT exposure builds steady tolerance in real life.
Many do both: EMDR first, then graded exposure. See: Overcoming Phobias with EMDR
OCD
**First line:**CBT with ERP.
Dialectical behavior therapy (DBT) is another therapeutic option that may benefit some individuals with OCD or related symptoms.
EMDR can help if trauma or sticky images fuel obsessions or if ERP stalls due to past events.
Read: EMDR for OCD
Depression & Low Self-Worth
CBT for activation, thought skills, routine rebuilds, and identifying and changing negative belief patterns.
EMDR for trauma-rooted shame or losses that “won’t move,” with a focus on recognizing and replacing negative beliefs linked to past events.
Grief support: EMDR for Grief & Loss.
Children & Teens
EMDR adapts well with drawings, play, tapping (less pressure to talk).
CBT teaches age-friendly skills for anxiety, school stress, and mood.
Explore: EMDR for Children & Teens.
Practical Fit: Time, Homework, Talking, and Cost
Timeframe: Single incident trauma can shift in 6–12 EMDR sessions; complex or multiple issues take longer. CBT timelines vary by goals and homework follow-through. EMDR can produce results faster than CBT, often requiring fewer sessions to see effects, especially when treating traumatic memories. EMDR is also used for conditions like PTSD, anxiety, and bipolar disorder.
**Homework load:**EMDR (lighter) vs. CBT (more reps).
Comfort: If talking details is hard, EMDR’s minimal narration may feel safer. If you like clear assignments, CBT may feel empowering.
Telehealth: Both work online with simple setups. Tips here: Telehealth EMDR.
Costs & insurance: Typical therapy rates apply; many plans cover both when clinically indicated. See our guide: How Much Is EMDR (2025) and local FAQ: Castle Rock EMDR FAQ.
“Your best therapy is the one you’ll actually do—and that fits your nervous system, schedule, and values”
Measuring Therapy Success
When you’re investing time and energy into therapy, it’s natural to wonder: “Is this working?” Measuring the success of EMDR therapy or CBT therapy is all about tracking real changes—like fewer PTSD symptoms, better daily functioning, and a stronger sense of well-being.
In the world of mental health, randomized controlled trials (RCTs) are the gold standard for figuring out what really helps. These studies compare different therapeutic approaches—like eye movement desensitization and reprocessing (EMDR) and cognitive behavioral therapy (CBT)—to see which ones are most effective for post traumatic stress disorder, anxiety disorders, obsessive compulsive disorder, eating disorders, and other mental health conditions. Thanks to decades of RCTs and meta-analyses, both EMDR and CBT are widely regarded as effective treatments for a broad range of mental disorders.
For EMDR therapy, success is often measured by how much traumatic symptoms decrease and how well you’re able to reprocess traumatic memories. EMDR therapists use tools like the Subjective Units of Disturbance (SUD) scale to track how distressing a memory feels, and the Validity of Cognition (VOC) scale to see how your beliefs about yourself shift as you heal. These measures help guide treatment planning and show when cognitive restructuring and emotional regulation are improving.
CBT therapy, on the other hand, focuses on changing negative thought patterns and unhelpful behaviors. CBT therapists use assessment tools that look at cognitive distortions, avoidance, and behavioral activation—basically, how your thinking and actions are shifting over time. Success in CBT is often seen in stronger coping strategies, less psychological distress, and more confidence handling daily challenges.
It’s important to remember that therapy isn’t one-size-fits-all. The best results come from a strong therapeutic relationship, a personalized treatment plan, and a willingness to try new coping strategies. Whether you’re working through traumatic experiences with desensitization and reprocessing EMDR, or tackling negative thoughts with cognitive behavioral therapy CBT, the goal is the same: to help you heal, grow, and reclaim your life from posttraumatic stress disorder and other mental health issues.
If you’re not sure which approach is right for you, a qualified mental health professional can help you weigh your options and measure your progress along the way. With the right support, both EMDR and CBT can be powerful tools for recovery and lasting change.
Can You Combine EMDR and CBT?
Absolutely. Common sequences:
EMDR → CBT: Clear the trauma jam first, then use CBT to rebuild habits, maintain gains, and practice real-world exposures.
CBT → EMDR: If skills help but a few triggers won't budge, target those memories with EMDR.
Parallel (alternating weeks): When scheduling and symptoms allow, especially for first responders/military (see: EMDR for Veterans & First Responders).
Quick Decision Checklist
Lean EMDR if you say:
“I keep seeing that image.”
“My body launches into panic out of nowhere.”
“I know it's over, but it doesn't feel over.”
“Talking it out hasn't moved it.”
Lean CBT if you say:
“I overthink everything and avoid a lot.”
“I need a plan and step-by-step habits.”
“I want skills for sleep, worry, social stuff.”
“I'm ready to practice exposures.”
Good-to-have therapist green flags:
Trained in your chosen modality (EMDRIA-trained for EMDR; CBT/ERP experience for anxiety/OCD).
Talks about safety, pacing, and fit (who benefits and who might not—see: Who Can Benefit & Who Cannot).
Offers a clear game plan and checks progress regularly.
We create education for a national audience and provide EMDR/CBT care across (in-person in Castle Rock ; secure telehealth statewide). If you're outside CO, find EMDR clinicians via EMDRIA's directory and CBT/ERP specialists via the IOCDF provider directory.
Browse related guides:
EMDR for PTSD • Anxiety • Panic • OCD • Phobias
FAQs: EMDR vs. CBT
Is EMDR “better” than CBT?Neither wins in all cases. EMDR tends to shine when symptoms are memory-driven; CBT excels when thought patterns and avoidance dominate. Many people benefit from both. In research comparing EMDR and CBT, studies use exclusion criteria to filter participants and ensure reliable results when assessing treatment effectiveness.
Do I have to talk through my trauma in detail with EMDR?No. EMDR can work with minimal narration and short, titrated sets. If speaking about details helps you, you can—but it’s not required.
What if I tried CBT and still feel stuck?That’s a common reason to add EMDR—especially if certain images or body jolts won’t budge. The reverse is true too: after EMDR, CBT helps rebuild routines and confidence.
Which works faster?For single-incident trauma, EMDR often moves faster. For skills goals (worry, sleep, social), CBT progress maps to your practice and exposure steps.
Is ERP always needed for OCD?For OCD, CBT with ERP is first-line. EMDR can help when PTSD/trauma complicates OCD or when ERP stalls due to past events. A dual-trained clinician will guide you.
Can kids do EMDR or CBT?Yes—both are adapted for age. EMDR uses play/drawing/tapping; CBT uses concrete, simple skills and family support. Read: EMDR for Children & Teens
Does online therapy work for EMDR and CBT?Yes. Telehealth EMDR uses taps/tones/onscreen tools; CBT translates easily to video. See our guide:
How many sessions will I need?It depends on goals and history. Some trauma cases shift in 6–12 EMDR sessions; CBT varies by condition and homework consistency. We’ll give a plan after intake.
Will insurance cover it?Often yes, when medically necessary and provided by a licensed clinician. Check your plan and our overview: How Much Is EMDR (2025).
Can I switch if my first choice doesn’t fit?Absolutely. Your plan should be adjustable. If you’re not improving within a reasonable window, your therapist should recommend a change in method or pacing.
Ready to talk through options? We’ll help you decide—no pressure, just clarity. If memories feel stuck, start with EMDR. If habits run the show, start with CBT. And if both are true…we’ll blend them so you can feel like you again. Reach out to us today for a free consultation.